In the world of oral health, there exists a silent intruder lurking beneath the surface, known as periodontitis – an advanced and serious form of gum disease. It’s a dental condition that can wreak havoc on your gums and teeth if left untreated, resulting in irreversible damage to your teeth gums, jawbone, and periodontium. Understanding its causes, symptoms, and treatment options is vital for optimal oral well-being.
Along the way, we’ll uncover the importance of periodontal maintenance and reveal the secrets to maintaining optimal oral hygiene. Additionally, we’ll explore the role of the best mouthwash for periodontal disease in your daily dental care routine.
What is Periodontitis?
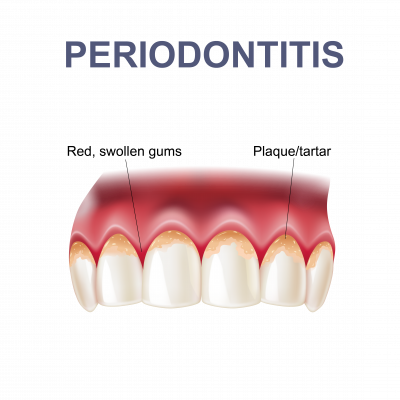
Periodontitis is a severe gum disease that affects the tissues and bones supporting the teeth, otherwise known as the periodontium. It occurs when bacteria in plaque irritate the gums, causing them to become inflamed. Initially, gum disease usually starts as gingivitis, a reversible condition, if left untreated, can lead to more serious complications, including periodontal abscess, irreversible bone and gum damage and eventually tooth mobility or even loss. Gum disease including periodontitis is also associated with various health conditions including cardiovascular diseases, Alzheimer’s, diabetes, and pregnancy-related complications.
By understanding the intricacies of this disease, you can take proactive steps toward maintaining optimal dental health. As always, preventing and managing periodontitis requires regular dental cleanings and proper oral hygiene.
Causes and Risk Factors
Let’s look at the key factors that trigger or increase the risk of periodontitis:

Inadequate Oral Hygiene
Poor dental hygiene practices, such as irregular brushing and flossing, can lead to the buildup of plaque, which can eventually cause periodontal disease. Periodontitis is often a result of untreated gingivitis which is usually reversible when treated early enough.
Smoking
Tobacco use is a significant risk factor for periodontitis. Smoking weakens the immune system and reduces the body’s ability to fight infections, including gum disease. This accelerates the accumulation of plaque and the formation of tartar or calculus, thereby acting as an inherent catalyst.
Genetic Factors
Some individuals may be more genetically predisposed to developing periodontal disease. Genetic variations can make them more susceptible to gum inflammation and tissue destruction, even among those with good oral hygiene.

Age
The risk of periodontitis increases with age. As we age, our bodies may become less effective at fighting off infections and maintaining oral health. It also becomes more difficult to effectively clean our teeth and gums which increases plaque accumulation and the risk of developing gum disease.
Some Health Conditions
Certain systemic conditions like diabetes, heart disease, and rheumatoid arthritis can increase the risk of periodontal disease. These conditions compromise the body’s immune system and can contribute to gum inflammation.
Symptoms
Periodontitis, also known as gum disease, can exhibit various symptoms. Often periodontitis is asymptomatic i.e., does not show symptoms until it has reached its moderate or advanced stages.
If you notice any of the following signs, it’s essential to consult your dentist for a proper diagnosis and treatment plan:

Inflamed or swollen gums: Periodontitis can cause your gums to become red, tender, and swollen.

Discoloured plaque or tartar on the teeth: The build-up of plaque and tartar or calculus can cause your teeth to appear yellow or brown.

Bleeding while brushing or flossing: Healthy gums should not bleed during oral hygiene practices, but gum bleeding can occur with periodontitis.

Halitosis, or bad breath: The bacteria in your mouth associated with periodontitis can produce foul-smelling odours.

Pain when eating or chewing: Periodontitis can lead to discomfort or pain when you bite or chew food. Bad breath

Sensitive teeth: As the gums recede, the roots of the teeth may become exposed, resulting in tooth sensitivity.

Loose teeth: In moderate and advanced periodontitis the supporting bone gum recede causing teeth to become mobile or loose.
If left untreated, periodontal disease advances through four stages. It initially starts with gingivitis, characterised by red, swollen gums, which can still be reversed with better oral care and regular dentist visits. The gums recede as they progress to mild periodontitis, leading to bone loss and pockets where bacteria thrive. Moderate periodontitis follows, causing more bone loss and discomfort. Finally, severe periodontitis can result in loose teeth, infections, and chronic bad breath.
Importantly, untreated periodontal disease is not just a dental issue; it’s linked to severe overall health problems like heart disease, stroke, and dementia.
Treatment
Treatment for periodontitis is critical to managing this oral health condition effectively. Due to its severity, periodontitis treatment is more invasive and involved than treatment for gingivitis. It is also important to note and based on the severity of periodontitis, your dentist may refer you to a periodontist, a specialist in periodontal treatment.
Nonsurgical Periodontitis Treatments
Nonsurgical periodontitis treatments are effective for mild to moderate cases. These are often completed at a general dental clinic by a dentist, dental hygienist, oral health therapist or in more severe cases by a gum specialist, periodontist:
- Antibiotics: Oral or topical antibiotics are prescribed to combat gum infection.
- Deep Scaling and Root Planing: A deep cleaning procedure involving local anaesthesia to remove bacteria from beneath the gums and smooth tooth roots.
- Home Oral Care: Your dental professional will educate you and recommend a variety of techniques and/or products to use at home to manage and prevent your gum disease progressing further.
- Ongoing Monitoring: Regular check-ups with your dental practitioner to evaluate the effectiveness of the treatment and maintain gum health.
Surgical Periodontitis Treatments
Surgical periodontitis treatments are necessary for moderate to severe cases and are performed by a periodontist, and include:
- Flap Surgery: A periodontist lifts gum tissue to access and thoroughly clean teeth roots. Bone re-contouring may be done if there’s bone loss.
- Dental Bone Grafts: Recommended for significant bone loss, this procedure involves placing grafting material in affected areas to support new bone growth.
- Gum Grafts: To address gum recession, gum graft surgery places tissue grafts around affected teeth, covering exposed tooth roots and improving aesthetics.
- Guided Tissue Regeneration: A biocompatible membrane is inserted to prevent unwanted tissue growth and encourage bone regeneration between existing bone and the tooth.
- Platelet-Rich Plasma (PRP): PRP derived from your blood is applied to deficient areas to stimulate the regeneration of bone and gum tissue.
Prevention
Prevention is critical when it comes to gum diseases. You can significantly reduce your risk of developing gum diseases like gingivitis and periodontitis by implementing simple habits into your daily routine.
Here are some steps you can take to prevent periodontitis:

Good Oral Hygiene
Maintaining a strict routine is essential in managing periodontitis. This includes brushing your teeth at least twice daily, flossing daily, and using mouthwash.

Use an Antimicrobial Mouthwash
Rinse with an antimicrobial mouthwash to help kill bacteria and reduce plaque buildup. Use PDS Chlorofluor (Chlorhexidine and Fluoride) Mouthwash.
Quit Smoking
Smoking is a significant risk factor for periodontal disease. Quitting smoking can improve your overall oral health.

Eat a Balanced Diet
A healthy diet of fruits, vegetables, and whole grains can help strengthen your immune system and prevent gum disease.

General Health
Maintain regular checkups with your doctor to help manage or prevent conditions which may increase your risk of developing gum disease. Always let your dental practitioner know should there be any changes to your health and/or if gum disease runs in the family.
Product Recommendations
Unleash the power of your smile with our Best Toothpaste for periodontitis! PDS Chlorofluor Toothpaste, a dental marvel, invigorates your oral hygiene routine. With its potent blend, it doesn’t just clean, it revitalises, fortifies, and rejuvenates your teeth. Experience the refreshing wave of dental excellence.
Best Toothpaste: PDS Chlorofluor Toothpaste (130g)
Unleash the power of your smile with our Best Toothpaste for periodontitis! PDS Chlorofluor Toothpaste, a dental marvel, invigorates your oral hygiene routine. With its potent blend, it doesn’t just clean, it revitalises, fortifies, and rejuvenates your teeth. Experience the refreshing wave of dental excellence.
Best Mouthwash: Curasept 0.20 Chlorhexidine with Fluoride Mouth Rinse (200ml)
Elevate your oral care with the Best Mouthwash for periodontitis! Curasept’s 0.20 Chlorhexidine with Fluoride Mouth Rinse is your daily dental elixir. It combines potency and protection, enveloping your mouth with a shield of freshness. Embrace the swish of confidence and health.
Best Gel: PDS 0.20 Chlorhexidine with Fluoride Gel (30ml)
Embrace the magic of our Best Gel for periodontitis! PDS 0.20 Chlorhexidine with Fluoride Gel is your secret weapon against oral adversaries. This potent elixir fortifies your defences, tackling dental challenges head-on. A small drop, a mighty impact.
Best Perio Kit: PDS Perio Pack (Chlorofluor Gel and Bright Teeth Whitening Gel)
Experience comprehensive dental care with PDS Perio Pack combines the strength of Chlorofluor Gel with the brilliance of this Teeth Whitening Gel. This dynamic duo enhances your oral care regimen, ensuring your smile shines as bright as your confidence.
Best Toothbrush: Caredent 10K Super Soft Toothbrush
Elevate your brushing experience with the Best Toothbrush! The Caredent 10K Super Soft Toothbrush is a dental masterpiece. Its ultra-soft bristles pamper your gums while effectively cleansing your teeth. Say goodbye to harsh brushing and hello to gentle excellence .
-
- Select options This product has multiple variants. The options may be chosen on the product page
$3.75 – $42.74 -
- Select options This product has multiple variants. The options may be chosen on the product page
-
- Select options This product has multiple variants. The options may be chosen on the product page
$16.99Original price was: $16.99.$15.99Current price is: $15.99. -
- Select options This product has multiple variants. The options may be chosen on the product page
$18.99Original price was: $18.99.$17.99Current price is: $17.99. -
- Select options This product has multiple variants. The options may be chosen on the product page
FAQs
Is Periodontitis Gum Disease?
Yes, Periodontitis is a form of gum disease. It’s a more advanced stage that involves inflammation and infection of the gums and the supporting structures of the teeth, including the bone. Not being treated can lead to serious damage and potentially even tooth loss. So, seeking dental care is essential if you suspect you have periodontitis to prevent further issues.
What Happens if Periodontal Disease Goes Untreated?
A variety of serious complications can occur including the formation of periodontal abscesses, bone loss, infections, tooth loss, bad breath, and even cardiovascular complications.
How Can I Reduce My Risk for Periodontitis?
You can reduce your risk by practicing good oral hygiene, quitting smoking, eating a balanced diet, and seeing your dentist and medical practitioners regularly for periodontal maintenance.
When Should I See a Dentist?
See a dentist for symptoms like inflamed gums, bleeding while brushing, flossing, or eating, sensitive teeth, tenderness when eating and loose teeth. Early intervention is critical in treating mild periodontitis and preventing further complications.